Photo from wikipedia
Simple Summary Esophageal and esophago-gastric junction adenocarcinomas (EA/EGJAs) are a heterogeneous group of cancers. Stage is the most important prognostic factor, while morphology, determined by histologic analysis, has up until… Click to show full abstract
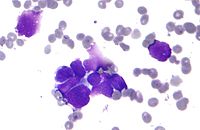
Simple Summary Esophageal and esophago-gastric junction adenocarcinomas (EA/EGJAs) are a heterogeneous group of cancers. Stage is the most important prognostic factor, while morphology, determined by histologic analysis, has up until now played a minor role. Even new molecular classifications (which should be based on accurate histologic assessment) are a long way off from being used in day to day practice. The reassessment of nearly 300 EA/EGJAs enabled us to re-evaluate morphology and identify a two-tiered grading approach in glandular adenocarcinomas (80%) based on a cut off of 6% of poorly differentiated components (well differentiated versus poorly differentiated). Furthermore, rare, but prognostically significant, variants were recognized with an in-depth morphologic description. On this basis, two morphologic risk groups (lower risk and higher risk) were identified, adding significant prognostic value to the stage. The accurate morphologic description of EA/EGJAs must be a prerequisite for a better understanding of prognosis, molecular events, and response to treatment. Abstract Stage significantly affects survival of esophageal and esophago-gastric junction adenocarcinomas (EA/EGJAs), however, limited evidence for the prognostic role of histologic subtypes is available. The aim of the study was to describe a morphologic approach to EA/EGJAs and assess its discriminating prognostic power. Histologic slides from 299 neoadjuvant treatment-naïve EA/EGJAs, resected in five European Centers, were retrospectively reviewed. Morphologic features were re-assessed and correlated with survival. In glandular adenocarcinomas (240/299 cases—80%), WHO grade and tumors with a poorly differentiated component ≥6% were the most discriminant factors for survival (both p < 0.0001), distinguishing glandular well-differentiated from poorly differentiated adenocarcinomas. Two prognostically different histologic groups were identified: the lower risk group, comprising glandular well-differentiated (34.4%) and rare variants, such as mucinous muconodular carcinoma (2.7%) and diffuse desmoplastic carcinoma (1.7%), versus the higher risk group, comprising the glandular poorly differentiated subtype (45.8%), including invasive mucinous carcinoma (5.7%), diffuse anaplastic carcinoma (3%), mixed carcinoma (6.7%) (CSS p < 0.0001, DFS p = 0.001). Stage (p < 0.0001), histologic groups (p = 0.001), age >72 years (p = 0.008), and vascular invasion (p = 0.015) were prognostically significant in the multivariate analysis. The combined evaluation of stage/histologic group identified 5-year cancer-specific survival ranging from 87.6% (stage II, lower risk) to 14% (stage IVA, higher risk). Detailed characterization of histologic subtypes contributes to EA/EGJA prognostic prediction.
Journal Title: Cancers
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!