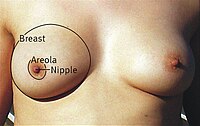
Photo from wikipedia
Simple Summary Patients with non-metastatic breast cancer may achieve partial or complete response after neoadjuvant treatment. Early response to treatment after two cycles of chemotherapy has been associated with complete… Click to show full abstract
Simple Summary Patients with non-metastatic breast cancer may achieve partial or complete response after neoadjuvant treatment. Early response to treatment after two cycles of chemotherapy has been associated with complete pathological response, longer disease-free interval and better overall survival. We aimed to investigate the role of morphologic, functional and relaxometry MR characteristics in predicting early response to neoadjuvant treatment. Tumor size, estrogen and progesterone receptors, HER2 status, Ki67%, tumor margins, enhancement type or ADC values were not associated with response. The T2 min relaxometry parameter and nodal stage were associated with early response, achieving an AUC of 0.826 [95% CI: 0.66–0.90, p-value < 0.001]. Abstract Aim: To evaluate the role of MR relaxometry and derived proton density analysis in the prediction of early treatment response after two cycles of neoadjuvant therapy (NAT), in patients with breast cancer. Methods: This was a prospective study that included 59 patients with breast cancer, who underwent breast MRI prior (MRI1) and after two cycles of NAT (MRI2). The MRI1 included a sequential acquisition with five different TE’s (50, 100, 150, 200 and 250 ms) and a TR of 5000 ms. Post-processing was used to obtain the T2 relaxometry map from the MR acquisition. The tumor was delineated and seven relaxometry and proton density parameters were extracted. Additional histopathology data, T2 features and ADC were included. The response to NAT was reported based on the MRI2 as responders: partial response (>30% decreased size) and complete response (no visible tumor stable disease (SD); and non-responders: stable disease or progression (>20% increased size). Statistics was done using Medcalc software. Results: There were 50 (79.3%) patients with response and 13 (20.7%) non-responders to NAT. Age, histologic type, “in situ” component, tumor grade, estrogen and progesterone receptors, ki67% proliferation index and HER2 status were not associated with NAT response (all p > 0.05). The nodal status (N) 0 was associated with early response, while N2 was associated with non-response (p = 0.005). The tumor (T) and metastatic (M) stage were not statistically significant associated with response (p > 0.05). The margins, size and ADC values were not associated with NAT response (p-value > 0.05). The T2 min relaxometry value was associated with response (p = 0.017); a cut-off value of 53.58 obtained 86% sensitivity (95% CI 73.3–94.2), 69.23 specificity (95% CI 38.6–90.9), with an AUC = 0.715 (p = 0.038). The combined model (T2 min and N stage) achieved an AUC of 0.826 [95% CI: 0.66–0.90, p-value < 0.001]. Conclusions: MR relaxometry may be a useful tool in predicting early treatment response to NAT in breast cancer patients.
Journal Title: Cancers
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!