Photo from wikipedia
Cerebral venous sinus thrombosis (CVST) is a rare cause of stroke that accounts for 0.5–1.0% of all strokes. Clinical presentation, predisposing factors, neuroimaging findings, and outcomes of CVST are extremely… Click to show full abstract
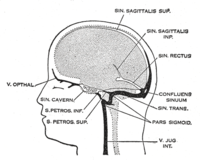
Cerebral venous sinus thrombosis (CVST) is a rare cause of stroke that accounts for 0.5–1.0% of all strokes. Clinical presentation, predisposing factors, neuroimaging findings, and outcomes of CVST are extremely diverse, which causes a high index of suspicion in diagnosis. Therefore, early diagnosis of CVST is crucial for prompt treatment to prevent morbidity and mortality. Objective: The purpose of this prospective study is aimed at assessing the clinical characteristics, potential risk factors, and neuro-radiological features along with the topography of venous sinus involved in CVST patients in a tertiary care hospital, Lahore, Pakistan. Material and Methods: Consecutive patients enrolled in this study had a computed tomography (CT) scan, magnetic resonance imaging (MRI), and magnetic resonance venography (MRV) along with a clinical presentation to confirm the diagnosis of CVST. Categorical data were presented as percentages. Continuous variable and categorical data were compared (parenchymal lesions vs. non-parenchymal lesions) using the Student’s t-test and Chi-square test, respectively. Results: A total of 3261 patients with stroke were presented during the study period. Out of all patients, 53 confirmed patients with CVST (1.6%) were recruited; the predominant population was female (84.91%), having a male to female ratio of 1:4. Mean age of the cohort was 28.39 ± 7.19 years. Most frequent symptoms observed were headache (92.45%) followed by vomiting (75.47%), seizures (62.26%), papilledema (54.72%), visual impairment (41.51%), and altered consciousness disturbance (52.83%). The presumed risk factors associated with CVST were puerperium (52.83%), use of oral contraceptives (13.21%), antiphospholipid syndrome (7.55%), elevated serum levels of protein C and S (5.66%), and CNS infection (3.77%). On cranial CT scans, 50 patients (94.33%) showed abnormalities while 32 patients exhibited various parenchymal lesions. Seizures were more frequent in CVST patients with parenchymal lesions compared with subjects lacking parenchymal lesions. Seventy-two sinuses, either single or in combination, were involved in CVST patients, being more common in patients with parenchymal lesions than those without parenchymal lesions. The most frequent locations of CVST were the superior sagittal and transverse sinus. Conclusion: In short, non-contrast CT brain may be used as a first line investigation in suspected cases of CVST. Our study also demonstrates some regional differences in the clinical features, risk factors, and neuroimaging details of CVST as described by some other studies. Therefore, care must be taken while diagnosing and predicting the outcome of the CVST.
Journal Title: Diagnostics
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!