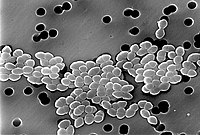
Photo from wikipedia
Previously it was shown that application of probiotics stopped the acquisition of vancomycin-resistant Enterococcus faecium (VRE) by patients in an early rehabilitation ward. Once the application of probiotics ended, we… Click to show full abstract
Previously it was shown that application of probiotics stopped the acquisition of vancomycin-resistant Enterococcus faecium (VRE) by patients in an early rehabilitation ward. Once the application of probiotics ended, we examined whether acquisition of VRE reoccurred. Furthermore, we examined whether probiotics altered prevalence of vancomycin-susceptible E. faecium (VSE) and Gram-negative bacteria, which produce extended spectrum beta-lactamase (ESBL). Although probiotic application ceased in April 2018, VRE-colonized patients rarely presented on that ward until 2019. Probiotic treatment also resulted in a decreased number of patients with VSE and ESBL. While decreased incidence of VRE occurred immediately, decreased VSE and ESBL numbers occurred months later. A probiotic-mediated decrease of VSE and ESBL incidence cannot be explained when assuming bacterial transmission exclusively as a linear cause and effect event. The decrease is better understood by considering bacterial transmissions to be stochastic events, which depend on various driving forces similar to an electric current. We hypothesize that VRE, VSE and ESBL uptake by patients and by staff members mutually reinforced each other, leading staff members to form a bacterial reservoir, similar to a condenser that stores electrical energy. Probiotic treatment then inhibited regeneration of that store, resulting in a breakdown of the driving force.
Journal Title: International Journal of Environmental Research and Public Health
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!