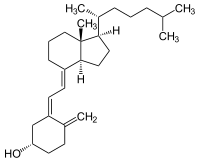
Photo from wikipedia
Poor vitamin D status has been associated with increased risk and severity of respiratory tract infections. Whether or not inflammation and infection affects 25-hydroxy vitamin D (25(OH)D) concentration is controversial… Click to show full abstract
Poor vitamin D status has been associated with increased risk and severity of respiratory tract infections. Whether or not inflammation and infection affects 25-hydroxy vitamin D (25(OH)D) concentration is controversial and is important in the interpretation of observational studies using plasma-25(OH)D as a biomarker for status. Our objectives were to measure whether 25(OH)D concentration was altered by an episode of acute lower respiratory tract infection and whether markers of inflammation predicted the 25(OH)D concentration. Children aged 2–35 months with severe (n = 43) and non-severe (n = 387) community-acquired, WHO-defined pneumonia were included. 25(OH)D concentration and inflammatory markers (cytokines, chemokines, and growth factors) were measured in plasma during the acute phase and 14, 45, and 90 days later. Predictors for 25(OH)D concentrations were identified in multiple linear regression models. Mean 25(OH)D concentration during the acute phase and after recovery (14, 45, and 90 days) was 84.4 nmol/L ± 33.6, and 80.6 ± 35.4, respectively. None of the inflammatory markers predicted 25(OH)D concentration in the multiple regression models. Age was the most important predictor for 25(OH)D concentration, and there were no differences in 25(OH)D concentrations during illness and after 14, 45, and 90 days when adjusting for age. Infection and inflammation did not alter the 25(OH)D concentration in young children with acute lower respiratory tract infections.
Journal Title: Nutrients
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!