Photo from wikipedia
Previously, we demonstrated that post-immunobiotics derived from Lactobacillus gasseri TMT36, TMT39, and TMT40 strains (HK36, HK39 and HK40, respectively) differentially regulated Toll-like receptor 3 (TLR3)-mediated antiviral respiratory immunity in infant… Click to show full abstract
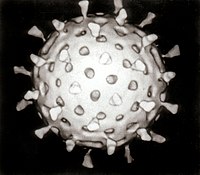
Previously, we demonstrated that post-immunobiotics derived from Lactobacillus gasseri TMT36, TMT39, and TMT40 strains (HK36, HK39 and HK40, respectively) differentially regulated Toll-like receptor 3 (TLR3)-mediated antiviral respiratory immunity in infant mice. In this work, we investigated whether the HK36, HK39 and HK40 nasal treatments were able to improve the resistance against primary respiratory syncytial virus (RSV) infection and secondary pneumococcal pneumonia. Our results demonstrated that the three treatments increased the resistance to primary viral infection by reducing variations in body weight, RSV titers and lung damage of infected infant mice. Post-immunobiotics significantly enhanced the expressions of interferon (IFN)-λ, IFN-β, IFN-γ, interleukin(IL) - 1β, IL-6, IL-27, Mx1, RNAseL and 2'-5'-oligoadenylate synthetase 1 (OAS1) genes and decreased tumour necrosis factor (TNF)-α in alveolar macrophages of RSV-challenged mice. In addition, the studies in the model of RSV-Streptococcus pneumoniae superinfection showed that the HK39 and HK40 treatments were capable of reducing lung damage, lung bacterial cell counts, and the dissemination of S. pneumoniae into the blood of infant mice. The protective effect was associated with increases in IFN-β, IFN-γ, IL-10, and IL-27 in the respiratory tract. This study demonstrates that the nasal application of the post-immunobiotics HK39 and HK40 stimulates innate respiratory immunity and enhances the defences against primary RSV infection and secondary pneumococcal pneumonia offering an alternative to combat respiratory superinfections in children, which can be fatal.
Journal Title: Beneficial microbes
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!