Photo from wikipedia
Objective: Congenital uterine anomalies are common; however, their effects on artificial insemination by husband (AIH) and the period during which AIH is converted to in vitro fertilization (IVF) are unclear.… Click to show full abstract
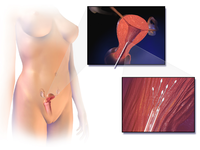
Objective: Congenital uterine anomalies are common; however, their effects on artificial insemination by husband (AIH) and the period during which AIH is converted to in vitro fertilization (IVF) are unclear. We examined the influence of uterine malformations on reproductive outcomes following AIH and the optimum number of AIH cycles before resorting to IVF-embryo transfer (IVF-ET). Methods: We retrospectively recruited 168 patients with uterine malformations (anomalous group) undergoing AIH between January 2011 and December 2016. Meanwhile, 168 patients with infertility but with normal uteri (normal group) were matched as controls according to age. Results: The clinical pregnancy rate was similar in both groups (12.4% vs. 12.3%, P = 0.950); the cancellation (21.6% vs. 4.4%, P < 0.001), early pregnancy loss (35.7% vs. 11.4%, P = 0.032), and preterm birth rates (21.4% vs. 2.9%, P = 0.038) were higher in the anomalous group, resulting in lower term birth (32.1% vs. 74.3%, P = 0.001) and live birth rates (50.0% vs. 77.1%, P = 0.034). After two AIH cycles, the clinical pregnancy rate was lower (3.6% vs. 23.1%, P = 0.037) among women with uterine anomalies than among those with normal uteri. There was no difference in the pregnancy rates (52.5% vs. 53.7%, P = 0.908) between the two groups of patients with unsuccessful AIH who then underwent IVF-ET. Conclusions: IVF-ET can be performed immediately after two unsuccessful AIH cycles in patients with uterine malformations. In patients undergoing AIH or IVF, uterine malformations increase the risk of adverse obstetric outcomes.
Journal Title: Reproductive and Developmental Medicine
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!