Photo from wikipedia
Introduction: Bioresorbable stent has the theoretical advantage in the pediatric age group; however, experience in the literature is very limited. Objectives: This pilot study sought to evaluate the feasibility, safety,… Click to show full abstract
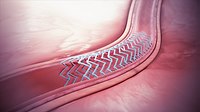
Introduction: Bioresorbable stent has the theoretical advantage in the pediatric age group; however, experience in the literature is very limited. Objectives: This pilot study sought to evaluate the feasibility, safety, and performance of iron bioresorbable scaffold (IBS Angel™) as short-term palliation in lesions with noncomplex patent ductus arteriosus (PDA). Materials and Methods: Nine neonates with duct dependent but dual-source pulmonary blood flow (PBF) were included. Major stent-related complications, in-hospital course, stent patency up to 6 months, and unplanned re-interventions were studied, as well the percentage of stent material resorbed in patients in whom the stents were explanted at the surgery. Results: IBS Angel™ was successfully implanted in all nine patients (mean weight range 3.4 ± 0.4 kg). Six were pulmonary atresia with an intact ventricular septum and 1 critical pulmonary stenosis patients where PDA stenting was done together or after balloon dilation. The mean procedure and fluoroscopy times were 89 ± 39 min and 16.3 ± 6.9 min, respectively. There were no major complications such as stent thrombosis or embolization and there were no in-hospital deaths. Post procedure overshunting and prolonged ventilatory support was a prominent feature. The median ventilation days was 3 (1–11 days). One patient died after 1 month due to respiratory syncytial virus pneumonia at the referring hospital. At 6 months follow-up, four had patent stents and four had blocked or restrictive stent flow. One patient received re-stenting at 4 months for restrictive stent flow. In three patients where microcomputed tomography of explanted stent was available, resorption of iron was 15% at 6 months and >65% at 16 months. Conclusions: Ductal stenting with IBS Angel™ is feasible and safe in selected patients. Because of early luminal loss, its use may be recommended for lesions with dual-source PBF with noncomplex PDA morphology that requires a short duration of palliation.
Journal Title: Annals of Pediatric Cardiology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!