Photo from wikipedia
Iron deficiency is the most widespread and frequent nutritional disorder in the world. It affects a high proportion of children and women in developing countries and is also significantly prevalent… Click to show full abstract
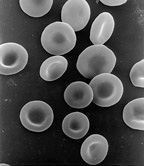
Iron deficiency is the most widespread and frequent nutritional disorder in the world. It affects a high proportion of children and women in developing countries and is also significantly prevalent in the industrialised world, with a clear predominance in adolescents and menstruating females. Iron is essential for optimal cognitive function and physical performance, not only as a binding site of oxygen but also as a critical constituent of many enzymes. Therefore iron deficiency at all its levels - nonanaemic iron deficiency, iron deficiency with microcytosis or hypochromia and iron deficiency anaemia - should be treated. In the presence of normal stores, however, preventative iron administration is inefficient, has side effects and seems to be harmful. In symptomatic patients with fatigue or in a population at risk for iron deficiency (adolescence, heavy or prolonged menstruation, high performance sport, vegetarian or vegan diet, eating disorder, underweight), a baseline set of blood tests including haemoglobin concentration, haematocrit, mean cellular volume, mean cellular haemoglobin, percentage of hypochromic erythrocytes and serum ferritin levels are important to monitor iron deficiency. To avoid false negative results (high ferritin levels in spite of iron deficiency), an acute phase reaction should be excluded by history and measurement of C-reactive protein. An algorithm leads through this diagnostic process and the decision making for a possible treatment. For healthy males and females aged >15 years, a ferritin cut-off of 30 µg/l is appropriate. For children from 6-12 years and younger adolescents from 12-15 years, cut-offs of 15 and 20 µg/l, respectively, are recommended. As a first step in treatment, counselling and oral iron therapy are usually combined. Integrating haem and free iron regularly into the diet, looking for enhancers and avoiding inhibitors of iron uptake is beneficial. In order to prevent reduced compliance, mainly as a result of gastrointestinal side effects of oral treatment, the use of preparations with reasonable but not excessive elemental iron content (28-50 mg) seems appropriate. Only in exceptional cases will an intravenous injection be necessary (e.g., concomitant disease needing urgent treatment, repeated failure of first-step therapy).To measure the success of treatment, the basic blood tests should be repeated after 8 to 10 weeks. Patients with repeatedly low ferritin will benefit from intermittent oral substitution to preserve iron stores and from long term follow-up, with the basic blood tests repeated every 6 or 12 months to monitor iron stores. Long-term daily oral or intravenous iron supplementation in the presence of normal or even high ferritin values is, however, not recommended and is potentially harmful.
Journal Title: Swiss medical weekly
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!