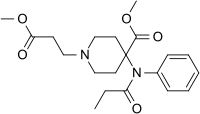
Photo from wikipedia
OBJECTIVE Characterize changes in intraoperative opioid and non-opioid administration over time and to evaluate self-reported pain scores in the immediate postoperative period. DESIGN Single-center retrospective longitudinal study. SETTING Academic medical… Click to show full abstract
OBJECTIVE Characterize changes in intraoperative opioid and non-opioid administration over time and to evaluate self-reported pain scores in the immediate postoperative period. DESIGN Single-center retrospective longitudinal study. SETTING Academic medical center. PATIENTS, PARTICIPANTS All patients presenting for surgery between 2011 and 2017 in both an inpatient and outpatient setting. MAIN OUTCOME MEASURE(S) Determine total intraoperative opioid administration using intravenous oral morphine equivalents standardized to weight and intraoperative non-opioid use. Furthermore, postoperative self-reported pain scores within 2 hours of completion of surgery are reported. RESULTS A total of 112,167 individual cases were identified from March 2011 to June 2017. There was a sustained and significant reduction in intraoperative mean and median opioid administration [2011: 0.16 ± 0.15 mg/kg and 0.13 (0-4.92) mg/kg vs 2017: 0.09 ± 0.09 mg/kg and 0.07 (0-4.17) mg/kg]. These effects are seen in emergent vs elective surgery, ambulatory vs inpatient, preoperative opioid use vs no preoperative opioid use, and those with and without intraoperative loco-regional procedures. Although median number of intraoperative non-opioid analgesic agents was unchanged over time, average difference in the number of intraoperative non-opioids increased over time. Finally, pain scores decreased over time [2011: mean (standard deviation) and median (range): 5.1 ± 2.62 and 5.4 (0-10) vs 2017: 3.29 ± 3.27 and 3 (0-10)]. CONCLUSION This study confirms that intraoperative opioid use has decreased over time with increased utilization of non-opioid analgesic adjuncts and a commensurate decrease in immediate postoperative pain.
Journal Title: Journal of opioid management
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!