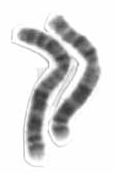
Photo from wikipedia
The titin gene (TTN), with its 364 exons, encodes the largest human protein. It gives rise to a dizzying array of alternatively spliced isoforms differentially expressed in various skeletal muscles,… Click to show full abstract
The titin gene (TTN), with its 364 exons, encodes the largest human protein. It gives rise to a dizzying array of alternatively spliced isoforms differentially expressed in various skeletal muscles, heart, and in development. Titin is not only the main spring element of the sarcomere, extending all the way from the Z-disc to the M-band, but it is also a stretch sensor and is involved in atrophy and other signaling pathways while interacting with a large and growing number of proteins, exerting many control and regulatory functions in muscles.1 No transcriptional unit exemplifies the unique diagnostic challenges posed by such a large and complex gene better than TTN. Until recently, the biggest challenge was to simply fully sequence TTN. Now, next-generation sequencing panels as well as whole-exome platforms have made TTN accessible to full-length testing on a routine basis. This development has rapidly increased diagnostic yields while amplifying the challenges posed by an increasingly large number of sequence variants of uncertain significance resulting from this high-throughput sequencing. These findings highlight the urgent need to confidently clarify the relevance of these variants. Savarese et al2 do an admirable job of illustrating and addressing these challenges. The discovery of the first skeletal muscle titinopathy caused by a mutation in the last exon in the M-band of TTN by Hackman et al3 in Finnish patients with dominant tibial muscular dystrophy (and its recessive occurrence as LGMD2J) was a titanic undertaking of manual sequencing.4 Laborious targeted exploration of the TTN sequence then resulted in the discovery of additional skeletal muscle TTN disorders, including hereditary myopathy with early respiratory failure,5 recessive tibial muscular dystrophy, and the recessive Salih myopathy with early cardiomyopathy.6 With next-generation sequencing facilitating easy surveillance of the entire TTN gene, mutations are now discovered at a much more accelerated pace. However, at the same time, variants of unknown significance in TTN are also emerging at an even faster pace while the understanding of the normal genomic landscape of TTN and its variations remain far from complete. This knowledge gap seriously hampers the proper assignment of pathogenicity of variants detected in a patient undergoing a diagnostic evaluation. Whilesometypesofvariants,suchasthosethatarepredicted toresult intruncation,seemconvincingasdisease-causingalleles at face value, others, including missense variants, are much less clear and pose the greatest challenge.7,8 While individually often rare, missense variants as a group are very common in the TTN gene. Unfortunately, in silico prediction of the effect of such variants currently is not very reliable forTTN. Furthermore, there is good evidence that there are mutations in TTN that are not detectable on currently used next-generation sequencing–based platforms (such as some deletions and duplications, inversions, or deep intronic mutations). These uncertainties can have significant consequences in that a titinopathy diagnosis may be either erroneously declared or prematurely discarded. Both scenarios can have consequences for genetic counseling, clinical management, and further diagnostic workup. It is therefore essential to be able to assign positive or negative plausibility to a titinopathy diagnosis, in particular if the TTN genotype found in the patient is incomplete or unresolved. Such scenarios arise when only 1 recessive variant has been detected when 2 would be expected; when there is 1 clear recessive variant, such as a truncation, but in compound heterozygosity with a rare missense variant of uncertain significance; and, perhaps most challenging, when only suspiciouslooking missense mutations are found. The diagnostic elements required for this plausibility process rely on the clinician as much as the geneticist, especially because approaching the diagnosis in this situation is an iterative process, returning to all available clinical, histological, genomic, and segregation data.9 Savarese et al2 demonstrate this process. They resequenced 504 undiagnosed patients on a next-generation multigene panel, identifying 9 newly confirmed and 4 potential patients with titinopathy carrying previously reported mutations (ie, hereditary myopathy with early respiratory failure– associated and tibial muscular dystrophy–associated mutations) as well as novel mutations. For recessively acting mutations, they identified clear biallelic truncations, and they also addressed the less obvious diagnostic scenarios outlined above. In particular, Savarese et al2 included patients with a missense variant in compound heterozygosity with a truncation, patients with an apparently missing second mutation, and patients with rare and potentially pathogenic missense variants on both alleles. The article puts forward a basic algorithm,2 outlining the elements involved to clarify such situations, which importantly also emphasizes the power of variant segregation studies in the family. In their approach, they also include Western blotting for TTN. This is an important addition to the diagnostic toolbox to show potential truncation at the protein level, which is currently only available on a research basis. An important point mentioned in this algorithm is that deep phenotyping needs to be an essential part in the diagnostic approach to support or disprove a diagnosis of titinopathy. Deep phenotyping as a diagnostic tool draws on the widening spectrum of manifestations associated with TTN mutations. This spectrum has expanded considerably since the routine use of next-generation sequencing and will continue to expand in particular for the recessive or, more accurately, biallelic cases (ie, some recessive skeletal muscle disease alleles may also be acting as dominant for conferring a risk for dilated cardiomyopathy10). The initial reports of recessive TTN disorders have mostly included only those patients with convincing biallelic mutations, which are predicted to be truncating mutations, and if a missense mutation was included, it had been worked up carefully for its functional effect.6,11,12 Related article page 557 Editorial Opinion
Journal Title: JAMA neurology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!